
In August 2020, CMS released proposed changes to Evaluation and Management (E&M) CPT codes. If approved, these changes would go into effect on January 1, 2021. While they are not finalized, these changes are significant enough to warrant the development of a plan to evaluate the impact on reported provider productivity and reimbursement.
Proposed Changes to Evaluation and Management Codes
CMS has proposed a two-fold change to E&M codes for 2021. First, the work component of the Relative Value Unit (wRVU) had been modified for CPT codes 99202-99205 and 99211-99215. CPT code 99201 would be removed completely. In addition to the updated wRVU value for these code ranges, CMS has also proposed a reduction to the conversion factor (CF) from $36.09 to $32.26. Overall, new patient visits would see a decrease in wRVUs while established visits would see an increase. The reduction of the conversion factor would apply to all CPT codes .
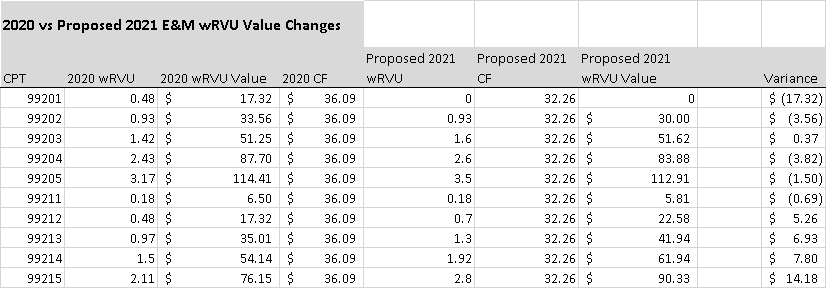
As noted in the chart above, the increased wRVU values for E&M codes primarily offset the reduction of the conversion factor for only established visits. New Patient E&M visits (99202-99205) would see an overall reduction in wRVU value. This is to be expected as the Department of Health and Human Services (HHS) requires that all changes to the Medicare Physician Fee Schedule (MPFS) be budget neutral therefore, any finalized changes, will result in increases in certain CPT codes with corresponding reductions in others. Professional organizations and medical specialty organizations are lobbying to ensure that any changes will have minimal negative impact to their respective parties.
wRVU vs Total RVU
It is also important to note the wRVU is only one component of the Total RVU value that ultimately determines Medicare Allowable.
The calculation to determine Medicare allowable is as follows:
[(GPCIw X wRVU)+ (GPCIpe x peRVU) + (GPCImp x mpRVU)] X CF = Allowable
The Geographic Practice Cost Index (GPCI) is a geographic adjustment to reimbursement which accounts for regional and practice-specific factors. Each state or region is assigned GPCI values which will determine the Medicare allowable rate for that area.
Implications to Provider Compensation
Anytime there a change to the CMS wRVU values or the Conversion Factor (and ultimately reimbursement), the review of provider compensation models and associated agreements is essential.
Considerations for physician reimbursement and compensation include Base Compensation, wRVU Thresholds, and Conversion Factors.
Most wRVU provider compensation models have a Base Salary component plus a wRVU related bonus. The provider is expected to produce a minimum number of wRVUs, or a Threshold, in exchange for set pay. Once a provider exceeds the Threshold, then a bonus would be calculated based on each additional wRVU produced. Typically, this would be the number of wRVUs produced beyond Threshold multiplied by a set dollar value, or Conversion Factor. The variations of this basic model are numerous and can be highly complex in nature. However, in most models, individually produced wRVUs and the corresponding Conversion Factor are still the key components.
Thresholds and Conversion Factors
The provider Threshold is often set on a combination of historical and expected productivity. Current provider compensation agreements will generally identify a minimum number of wRVUs that represent a specific number of visits or procedures. Likewise, the CMS Conversion Factor determines the value of this productivity and therefore the expected reimbursement. Herein lies the rub. The new wRVU values and associated CF proposed by CMS will change the value of the work component and possibly overall reimbursement for the same services. So, providers could be generating more or less revenue for the exact same work and it may no longer accurately be reflected by their current compensation based on individual code frequency.
Example:
Taking into account the 2021 GPCI values for the Alabama Region, this chart identifies the difference in reimbursement for the same 100 visits. Should the proposed changes be approved, the presented services would be reimbursed 3.73% higher in 2021 compared to 2020 for the same work.
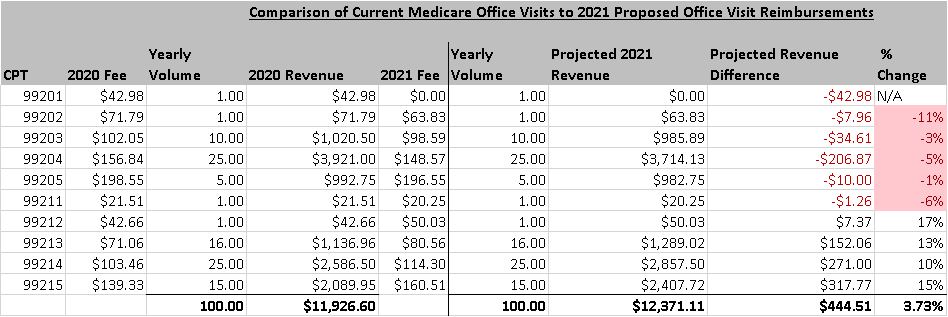
Extrapolation of the comparison above to an entire year may result in significant variance.
Additionally, while the wRVU values may not change for non E&M codes, the reduction in the CMS conversion factor alone would prove impactful.
Benchmarking
Intrinsic to practice management is the ability to compare the Key Performance Indicators (KPI) to other like practices as well as historical data. There are several sources for practice benchmarking, with MGMA Datadive being often referenced. The proposed changes to wRVU values and the CMS conversion factor will render many benchmarks unsuitable for comparison. Benchmarks require a comparison of equal data points to be truly valid. Therefore, KPIs including, productivity metrics, revenue data and wRVU statistics will be based on different data standards and may not be comparable to previous years’ benchmarks.
Final Thoughts
It is important to remember that these changes are proposed and not final. Even if approved, these proposals could undergo additional modifications prior to the release of the final rule. At this time, health organizations should be analyzing how theses changes could affect overall revenue. Equally important is the recognition of any potential impact to the measurement of provider productivity and the translation of those changes to provider compensation.
Kassouf to host 22-annual medical coding workshop

Kassouf director named one of the nation’s best financial planners

